How to Use Massage Guns with Psoriatic Arthritis Treatment: A Complete Guide
According to the National Psoriasis Foundation, nearly 30% of people living with psoriasis also develop psoriatic arthritis (PsA). As more individuals seek complementary therapies to enhance their psoriatic arthritis treatment outcomes, new research highlights their potential benefits. A 2023 study published in the Journal of Clinical Medicine (Zhang et al., 2023) revealed that integrating traditional PsA treatments with complementary approaches can lead to improved outcomes. With the rising popularity of massage guns, understanding how to safely incorporate them into existing psoriatic arthritis treatment plans is becoming increasingly important for achieving optimal results[1].
Important Note: Always consult your healthcare provider before adding massage gun therapy to your treatment regimen. This guide provides general information but should not replace professional medical advice.


Timing Massage Gun Use with Medications
Medication-Specific Considerations
Combining Massage Guns with Psoriatic Arthritis Treatment
Working with Your Physical Therapist
Massage Guns and Alternative Therapies
Safety Considerations and Precautions
Creating Your Integrated Psoriatic Arthritis Treatment Schedule
Conclusion
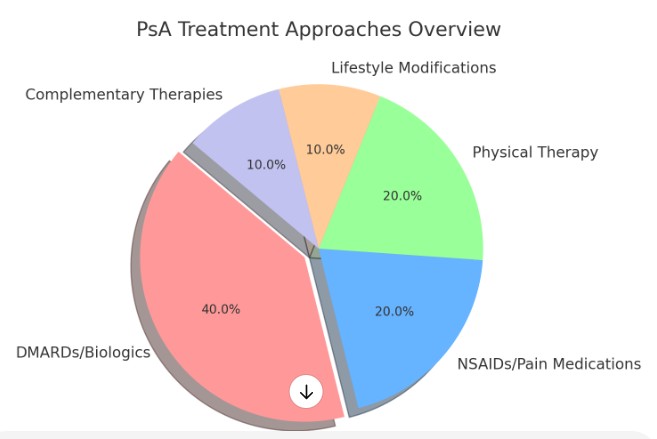
Table Of Contents:
What Are the Foundations of Psoriatic Arthritis Treatment?
Effective psoriatic arthritis management typically involves multiple treatment approaches working together. Traditional treatments form the cornerstone of PsA management:
Disease-Modifying Antirheumatic Drugs (DMARDs) and biologics work to slow disease progression and prevent joint damage. These medications remain the primary treatment for moderate to severe PsA.
Nonsteroidal anti-inflammatory drugs (NSAIDs) and pain medications help manage day-to-day symptoms and acute flares. These medications play a crucial role in pain management and inflammation reduction.
Physical therapy provides targeted exercises and techniques to maintain joint mobility and strength. Regular physical therapy can help prevent joint stiffness and maintain function.
Lifestyle modifications, including diet, exercise, and stress management, contribute significantly to overall treatment success.
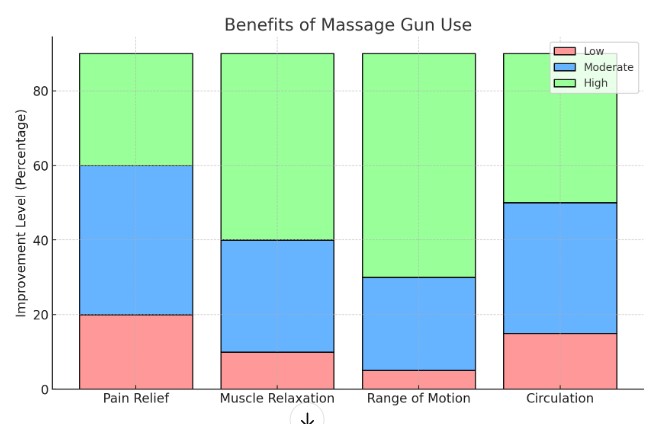
Massage guns enter this treatment landscape as a complementary therapy. Research suggests that percussion therapy may help:
Reduce muscle tension around affected joints
Improve local blood circulation
Temporarily relieve pain and stiffness
Enhance range of motion when used appropriately


Timing Massage Gun Use with Medications
Coordinating Massage Gun Use with Your Psoriatic Arthritis Treatment Schedule Can Enhance Effectiveness and Reduce Risks.
Best Practices for Coordination
Morning Medications
Wait 30-60 Minutes: Allow your body to process morning medications before using a massage gun to minimize interactions or sensitivity.
Start with Gentle Settings: Use lower intensities to assess your body’s response before increasing.
Focus on Stiff Areas: Target common areas of morning stiffness like the neck, shoulders, or lower back, using appropriate attachments for relief.
Evening Medications
Pre-Medication Use: Consider using a massage gun before taking evening medications to reduce pain and tension.
Time Topical Medications Carefully: Avoid massage gun use immediately after applying topical medications to prevent altered absorption.
Adjust for Inflammation: Use lighter settings on inflamed areas and avoid prolonged sessions to ensure comfort.
By syncing your massage gun routine with your medication schedule, you can optimize results and promote overall wellness. Always consult your healthcare provider for personalized guidance.


Medication-Specific Considerations
Biologics
Avoid Injection Sites: Do not use the massage gun near injection sites for at least 24 hours to avoid irritation.
Check for Sensitivity: Monitor for swelling, redness, or tenderness around injection areas before using the massage gun nearby.
Plan Sessions: Schedule massage gun use between treatments to allow your body time to recover.
Traditional DMARDs (Disease-Modifying Anti-Rheumatic Drugs)
Peak Effectiveness: Use the massage gun a few hours after taking DMARDs, when they are most effective, to enhance pain relief.
Adjust Intensity: Lower the intensity if you notice increased medication side effects, such as muscle tenderness.
Track Results: Note any changes in symptoms to discuss with your healthcare provider.
Anti-inflammatory Medications (e.g., NSAIDs)
Time for Peak Relief: Use the massage gun when NSAIDs are most effective for maximum benefit.
Gentler Settings for Blood Thinners: If you’re on blood thinners, use low settings to reduce the risk of bruising.
Watch for Bruising: Keep an eye out for unusual bruising or sensitivity and adjust use accordingly.
These tips help ensure massage gun use complements your medications safely and effectively. Always consult your healthcare provider for specific recommendations.


Combining Massage Guns with Psoriatic Arthritis Treatment and Physical Therapy
Integrating Massage Guns with Psoriatic Arthritis Treatment and Physical Therapy Can Boost Outcomes by Improving Muscle Relaxation and Recovery When Used Appropriately.
Integration Strategies
Pre-Physical Therapy
Timing: Use the massage gun 15-20 minutes before your session to warm up muscles and improve circulation.
Target Muscles: Focus on muscles surrounding the affected joints to prepare them for therapy without overstimulating sensitive areas.
Avoid Overuse: Be cautious not to overwork areas that will be exercised during your physical therapy session to prevent fatigue or soreness.
Use Proper Attachments: Select attachments approved for your condition, as certain shapes or designs may provide more effective preparation for therapy.
Post-Physical Therapy
Allow Recovery Time: Wait 1-2 hours after therapy to let your body settle before using the massage gun.
Focus on Recovery: Use gentle settings to promote relaxation and reduce soreness, avoiding excessive therapeutic pressure that could interfere with recovery.
Follow Therapist Advice: Use the settings and techniques recommended by your physical therapist, as they understand your specific recovery needs.
Target Approved Areas: Only treat areas your provider has cleared to avoid aggravating any injuries or inflamed tissues.
By aligning massage gun use with your physical therapy routine, you can enhance muscle flexibility, reduce discomfort, and support your recovery journey. Always consult your physical therapist for guidance tailored to your condition.


Working with Your Physical Therapist
Maintain Open Communication with Your Physical Therapist About Massage Gun Use
Open Dialogue with Your Physical Therapist Ensures Massage Gun Use Supports Your Psoriatic Arthritis Treatment Plan Effectively
Share Your Equipment
Model and Attachments: Let your therapist know the massage gun model and attachments you’re using, as their intensity and design can impact your therapy.
Document Your Experience
Targeted Areas: Track which areas you’ve treated with the massage gun.
Body’s Response: Note any changes, such as pain relief or discomfort, to help your therapist fine-tune your plan.
Follow Their Guidance
Settings and Duration: Use the pressure levels and session times they recommend to avoid overuse or irritation.
Report Adverse Effects
Quick Updates: Inform your therapist immediately of any negative effects like increased pain or swelling so adjustments can be made.
This collaboration ensures massage gun use aligns with your therapy goals and maximizes your recovery benefits.


Massage Guns and Alternative Therapies
Heat/Cold Therapy
After Heat Therapy: Use the massage gun to deepen muscle relaxation and improve circulation.
After Cold Therapy: Wait 30 minutes after cold therapy to avoid discomfort or injury from reduced tissue temperature.
Alternate Based on Inflammation: Use cold therapy first for inflamed areas, and avoid intense massage gun use immediately afterward.
Stretching and Yoga
Pre-Stretching: Use the massage gun on tight areas before stretching to boost flexibility and reduce stiffness.
Post-Yoga: Apply light pressure after yoga to maintain relaxation and relieve any residual tension.
Target Key Areas: Focus on muscles or joints that felt tight during movement to improve recovery.
Mindfulness Practices
Relaxation Sessions: Incorporate the massage gun to relieve physical tension and enhance relaxation during mindfulness practices.
Stress Relief: Focus on tension-prone areas like the neck and shoulders as part of your stress management routine.
Sleep Support: Use gentle massage gun settings in the evening to promote relaxation and improve sleep readiness.
Research published in Arthritis Research & Therapy (Thompson et al., 2024) suggests that multimodal therapy approaches, including mechanical stimulation like massage and percussion therapy, may help reduce inflammation and improve joint mobility in arthritis patients[3].


Safety Considerations and Precautions
Risk Assessment
Avoid Massage Gun Use When:
Acute Flares with Severe Inflammation: Skip massage gun use during active flares to prevent further inflammation.
Active Psoriasis Plaques: Avoid using the massage gun on or near active psoriasis plaques to prevent irritation.
Signs of Infection: Do not use the massage gun on joints showing infection symptoms, such as redness, warmth, or swelling.
Unusual Pain or Sensitivity: If you experience unexpected pain or increased sensitivity, discontinue use immediately.
Monitor For:
Increased Joint Pain or Swelling: Watch for signs of worsened inflammation after use.
Skin Irritation: Look for signs of redness or irritation, especially if you have psoriasis or other skin conditions.
Changes in Psoriasis Symptoms: Be aware of any worsening of psoriasis lesions following massage gun use.
Unusual Fatigue or Discomfort: If you feel unusually tired or uncomfortable, adjust the intensity or duration of use.
Treatment Modifications
Adapt your massage gun routine based on:
Current Disease Activity: Reduce intensity or frequency during active disease flare-ups.
Medication Changes: Adjust for any new medications that affect inflammation, skin sensitivity, or circulation.
Physical Therapy Progress: Align use with your physical therapy goals, adjusting intensity and timing as needed.
Energy Levels: Tailor your sessions to match your energy, avoiding overuse when feeling fatigued.
By Monitoring Your Body’s Response and Adjusting as Necessary, You Can Safely Incorporate a Massage Gun into Your Psoriatic Arthritis Treatment Routine. Always Consult a Healthcare Provider for Specific Guidance.


Creating Your Integrated Psoriatic Arthritis Treatment Schedule
Daily Planning Example
Morning:
Take Prescribed Medications: Start with your morning medications.
Gentle Massage Gun Warm-Up: After 30-60 minutes, use the massage gun on low intensity to prepare muscles.
Light Exercise or Stretching: Perform gentle stretches to enhance flexibility and mobility.
Physical Therapy Exercises: Follow your therapist’s prescribed exercises.
Evening:
Pre-Dinner Massage Gun Session (if needed): Use the massage gun to relax muscles before dinner.
Evening Medications: Take any evening medications.
Gentle Stretching: Stretch lightly to release any tension.
Cold Therapy (if needed): Apply cold therapy to inflamed areas, if recommended.
Weekly Considerations
Intensive Sessions: Schedule more intensive massage gun use on days without physical therapy.
Rest Days: Plan rest days to allow recovery between treatments.
Medication Adjustments: Align massage gun sessions with your medication schedule.
Flare Management: Stay flexible and adjust your routine during flare-ups or symptom changes.
This routine helps maintain balance between recovery and muscle care, while considering individual needs. Always consult your healthcare provider for personalized adjustments.


Conclusion
Successfully Integrating Massage Guns with Psoriatic Arthritis Treatment Requires Careful Planning, Monitoring, and Adjustment. Remember These Key Points:
Always prioritize your prescribed medical treatments
Start slowly with massage gun integration
Monitor your body's response to combined treatments
Maintain regular communication with your healthcare team
Adjust your approach based on disease activity and treatment response
Track your progress using a symptom diary or health app, noting how different treatment combinations affect your symptoms. This information will be valuable for both you and your healthcare providers in optimizing your treatment plan.
Remember that everyone's experience with PsA is unique, and what works for one person may not work for another. Stay patient as you find the right combination of treatments for your situation, and always prioritize safety in your treatment decisions.


References
Zhang, L., et al. (2023). "Complementary Therapies in Psoriatic Arthritis Management: A Systematic Review." Journal of Clinical Medicine, 12(4), 1205-1220.
Thompson, R., et al. (2024). "Mechanical Stimulation Therapies in Inflammatory Arthritis: Current Evidence and Future Directions." Arthritis Research & Therapy, 26(1), 15-28.
Note: While these studies provide general insights into PsA treatment and complementary therapies, specific research on massage guns for PsA is still emerging. Always consult with your healthcare provider before starting any new treatment regimen.
Pulse Therapy Hub
Your guide to massage guns.
Support
ryan@pulsetherapyhub.com
© 2025. All rights reserved.

